
Connection. Advocacy. Growth.

You may earn this many credits: 6.5
Insomnia is widely recognized to be the most common sleep problem and is also a leading complaint in primary care settings. The consequences and morbidity associated with chronic insomnia can be substantial across several domains and can include increased health care utilization, impaired quality of life, increased risk of falls and hip fractures, increased risk of medical and psychiatric disorders, and ultimately worse outcomes for all co-morbid disorders.
Effective treatment of insomnia not only improves sleep quality and daytime functioning, but also may improve comorbid conditions such as chronic pain and depression. In particular, cognitive-behavioral treatments for insomnia have been shown to be of equal or greater effectiveness when compared to sedative hypnotic medication.
This workshop is designed to provide clinical and research faculty from multiple disciplines the core elements of cognitive-behavioral treatment for insomnia. The course starts by grounding participants in the basics of sleep medicine that undergird the practice of CBT-I. It goes on to present systematic, empirically validated treatment methods and essential information about the etiology and evolution of chronic insomnia necessary to inform assessment, diagnosis, treatment, and the handling of treatment resistance.
Objective 1
Define the basics of sleep nomenclature including sleep period, phase, continuity, and architecture.
Objective 2
Define and distinguish acute insomnia from insomnia disorder and discuss the importance of treating the chronic form as a specifically targeted comorbidity.
Objective 3
Cite the evidence for the efficacy of CBT-I for both primary and co-morbid insomnia disorder.
Objective 4
Explain the Spielman model of insomnia and basics of sleep regulation, and demonstrate how to utilize these concepts in the deployment of CBT-I.
Objective 5
Explain how to obtain useable patient sleep diary data, and how to analyze the data for use in the course of CBT-I treatment.
Objective 6
Apply the techniques of stimulus control and sleep restriction therapy to the treatment of chronic insomnia.
Objective 7
Apply the techniques of sleep hygiene education and cognitive therapeutic strategies to the treatment of chronic insomnia.
Objective 8
Apply a decision-making algorithm to case conceptualization, and explain the steps necessary to aide in good relapse prevention.
The VPA Psychological Association is approved by the American Psychological Association to sponsor continuing education for psychologists. The VPA Psychological Association maintains responsibility for this program and its content.
| Research References | Available after Purchase | ||
| Presentation Slides (14.57 MB) | 80 Pages | Available after Purchase |
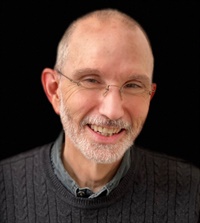
Dr. Donn Posner is the Founder and President of Sleepwell Consultants and has been consulting to organizations and individuals on a wide variety of sleep health issues including insomnia, circadian dysrhythmia, CPAP adherence, and parasomnias. He is also currently an Adjunct Clinical Associate Professor in the Department of Psychiatry and Behavioral Sciences at the Stanford University School of Medicine and a consulting psychologist for the Palo Alto VA. Dr. Posner is currently working on a number of grants exploring the effects of CBT-I in Gulf War veterans, and veterans with insomnia and Mild Traumatic Brain Injury. He is also working on a pilot aimed at using CBT-I techniques to decrease fatigue in breast cancer survivors by increasing total sleep time.
Prior to this he spent 25 years serving as the Director of Behavioral Sleep Medicine for the Sleep Disorders Center of Lifespan Hospitals, and was a Clinical Associate Professor in the Department of Psychiatry and Human Behavior at the Warren Alpert School of Medicine at Brown University. Dr. Posner is a member of the American Academy of Sleep Medicine and is one of the first Certified Behavioral Sleep Medicine specialists recognized by that group. He is also a founding member of the Society of Behavioral Sleep Medicine and he has also now achieved the status of Diplomate with the Board of Behavioral Sleep Medicine (BBSM).